radioiodine therapy (low dose)
What is Radioiodine Therapy (Low Dose)?
Radioiodine therapy (low dose) uses a small amount of radioactive iodine-131 (I-131) to manage thyroid-related conditions, particularly overactive thyroid (hyperthyroidism) and certain types of thyroid nodules. The therapy involves taking a capsule or liquid form of I-131, which the thyroid gland absorbs. The radioactive iodine selectively destroys overactive thyroid tissue while preserving normal thyroid function as much as possible.
Since the thyroid naturally takes up iodine, this targeted therapy minimises exposure to other organs. A low dose of radioiodine is generally used for milder cases, reducing the risk of side effects while still being effective.
Who is Suitable for Radioiodine Therapy (Low Dose)?
A low-dose radioiodine therapy may be recommended for individuals with the following conditions:
- Mild to moderate hyperthyroidism – Including conditions such as Graves’ disease or toxic multinodular goitre.
- Thyroid nodules – Some non-cancerous thyroid nodules that produce excess hormones can be treated with low-dose radioiodine.
- Patients who do not respond well to antithyroid medications – If medications such as carbimazole or propylthiouracil are ineffective or cause side effects, radioiodine therapy may be an alternative.
- Elderly patients or those with comorbidities – For individuals who may not be suitable candidates for surgery, radioiodine therapy provides a non-invasive alternative.
- Patients seeking a non-surgical approach – Those who prefer a less invasive treatment than thyroid surgery.
However, this therapy is not recommended for:
- Pregnant or breastfeeding women, as the radioactive iodine, can affect the developing baby or pass into breast milk.
- Patients with severe thyroid eye disease (in cases of Graves’ disease), as it may worsen eye symptoms.
Benefits of Radioiodine Therapy (Low Dose)
- Effective and long-lasting – A single treatment can provide permanent control of hyperthyroidism in most cases.
- Non-invasive – Unlike surgery, no incisions, scars, or anesthesia risks exist.
- Targeted action – The iodine is selectively absorbed by thyroid cells, minimising damage to surrounding tissues.
- Minimal side effects – Compared to higher doses, low-dose therapy has fewer adverse effects, such as hypothyroidism.
- Convenient treatment – The procedure is simple, usually requiring just one dose, and is outpatient.
- Alternative to medication – Some patients experience side effects or require lifelong medication, making radioiodine therapy a more sustainable solution.
Conditions Treated by Radioiodine Therapy (Low Dose)
Conditions that may be identified and subsequently treated with low-dose radioiodine therapy include:
- Graves' Disease – An autoimmune disorder causing hyperthyroidism.
- Toxic Multinodular Goiter – An enlarged thyroid with multiple hormone-producing nodules.
- Toxic Adenoma – A single overactive thyroid nodule.
- Subclinical Hyperthyroidism – Mildly elevated thyroid hormone levels that may progress to more severe hyperthyroidism.
Preparation for Radioiodine Therapy (Low Dose)
Proper preparation helps ensure precise and accurate images. Here’s what you need to know:
Radioiodine Therapy Preparation Summary
- 1 hour
- Preparation will be given at booking time
What to Bring
- Referral Letter – Required for hospital or clinic documentation.
- List of Medications – Include any prescription and over-the-counter medications.
What to Wear
- Loose-fitting clothing is ideal.
- Avoid metal accessories, as you may be asked to remove them.
Dietary Restrictions Before Therapy
- Low-Iodine Diet (1-2 Weeks Before Treatment) – This helps increase iodine absorption during therapy. Avoid:
- Dairy products
- Seafood and seaweed
- Iodised salt
- Egg yolks
- Processed foods with added iodine
Medication Adjustments
- Thyroid Medications – Your doctor may ask you to stop or adjust antithyroid medications like methimazole or carbimazole a few days before therapy.
- Other Medications – Some medications can interfere with iodine absorption, so your doctor will advise which ones to stop temporarily.
How Long Does the Procedure Take?
- The therapy is quick and painless, typically taking 15 to 30 minutes.
Radioiodine Therapy (Low Dose) Procedure
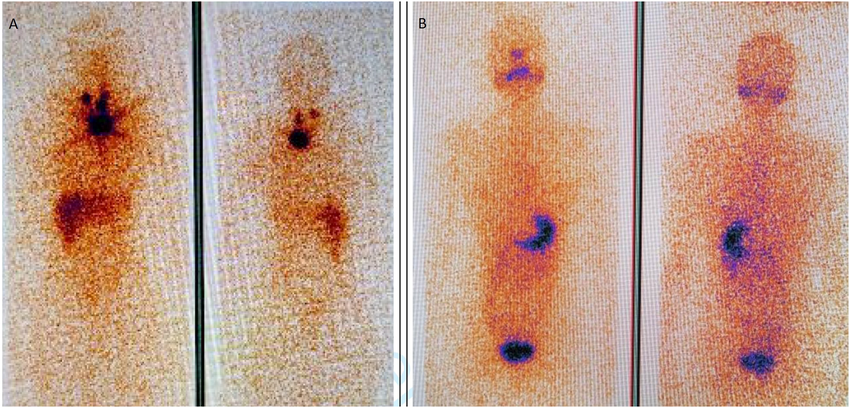
- Consultation and Confirmation: The medical team will review your medical history and confirm that the therapy is appropriate. A thyroid uptake scan may have been performed to determine how much iodine your thyroid absorbs.
- Administration of Radioiodine: You will be given a capsule or liquid form of iodine-131 (I-131) to swallow. The radioiodine is odorless and tasteless. You will be instructed to drink plenty of water to help the absorption process.
- Discharge and Home Isolation Instructions: Most patients can go home the same day. Specific radiation safety precautions will be provided to minimise exposure to others.
What to Expect After a Radioiodine Therapy (Low Dose)?
After radioiodine therapy, your body will release small amounts of radiation for a short period. To ensure safety and effective recovery, follow these instructions:
Radiation Safety Precautions (For 3-7 Days)
- Avoid Close Contact – Stay at least one meter away from others, especially children and pregnant women.
- Sleep Alone – If possible, use a separate bed.
- Limit Physical Contact – Avoid kissing, hugging, or prolonged close interactions.
- Flush Twice – After using the toilet, wash your hands twice.
- Use Separate Utensils – Do not share cutlery, cups, or food with others.
- Wash Clothes Separately – Laundry should be washed separately from others' clothes.
Diet and Hydration
- Increase Fluid Intake – Drink plenty of water to help flush excess radioiodine from your system.
- Resume Normal Diet – You can return to your regular diet unless otherwise advised.
Follow-Up Appointments
- You will need thyroid function tests 4 to 6 weeks after therapy to assess its effectiveness.
- Your doctor will determine if additional treatments, such as thyroid hormone replacement, are necessary.
Radioiodine Therapy (Low Dose) Prognosis
The prognosis after low-dose radioiodine therapy is generally excellent, with many patients achieving long-term control of their thyroid condition. The treatment effectively reduces thyroid hormone production while minimising side effects. However, the outcome varies depending on the underlying condition:
- Hyperthyroidism (Graves’ Disease, Toxic Nodules, Multinodular Goiter)
- Most patients see improvement within 4 to 8 weeks after treatment.
- In many cases, hyperthyroidism is completely resolved after one treatment.
- Some patients may require a second dose if thyroid hormone levels remain elevated.
- There is a 20-50% chance of developing hypothyroidism (underactive thyroid), requiring lifelong thyroid hormone replacement therapy.
- Benign Thyroid Nodules
- Nodules usually shrink over several months.
- Symptoms such as neck discomfort or pressure improve gradually.
- Long-Term Outlook
- Most patients require regular thyroid function tests every 6 to 12 months.
- If hypothyroidism develops, it is easily managed with levothyroxine (thyroid hormone replacement).
- Patients generally return to normal activities within a few days after treatment.
Radioiodine Therapy (Low Dose) Risks
Short-Term Risks
- Mild Neck Pain or Swelling – A temporary inflammatory response can cause slight discomfort.
- Nausea – Some patients experience mild nausea shortly after ingestion.
- Dry Mouth or Altered Taste – Radioiodine can affect the salivary glands, leading to temporary dryness or metallic taste.
Long-Term Risks
- Hypothyroidism (Underactive Thyroid)
- Worsening of Thyroid Eye Disease
- Reduced Fertility (Temporary in Men)
- Minimal Radiation Exposure to Others
What if Radioiodine Therapy (Low Dose) is Delayed?
Delaying treatment depends on the severity of the thyroid condition. Potential consequences include:
For Hyperthyroidism
- Persistent Symptoms – Weight loss, palpitations, anxiety, and heat intolerance may continue or worsen.
- Heart Problems – Untreated hyperthyroidism can increase the risk of atrial fibrillation (irregular heartbeat) and heart failure.
- Osteoporosis – Prolonged high thyroid hormone levels weaken bones, increasing fracture risk.
For Thyroid Nodules
- Nodule Growth – If left untreated, nodules may enlarge, leading to difficulty swallowing or breathing.
- Increased Hyperthyroidism Risk – Some nodules may start overproducing thyroid hormones, worsening symptoms.
For Graves’ Disease
- Progression of Thyroid Eye Disease – Delaying treatment for Graves’ disease may allow eye symptoms to worsen, including bulging eyes and vision issues.
Radioiodine Therapy (Low Dose) Costs
- Medicare-Covered: Bulk billed. No out-of-pocket cost.