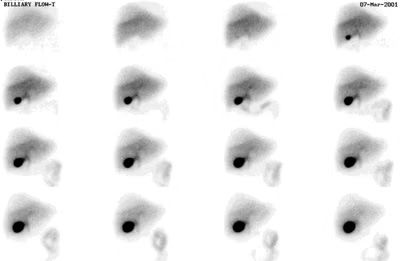
hepatobiliary scan
What is a Hepatobiliary Scan?
A hepatobiliary scan, also known as a HIDA scan (hepatobiliary iminodiacetic acid scan), is a nuclear medicine imaging test used to evaluate the function of the liver, gallbladder, and bile ducts. This scan shows how well the gallbladder is working or, if you have already had your gallbladder removed, if there are any blockages in the bile duct.
Who is Suitable for a Hepatobiliary Scan?
A hepatobiliary scan is recommended for individuals experiencing symptoms of gallbladder disease or bile duct obstruction. It is often used when other imaging tests, such as ultrasound or CT scans, do not provide a clear diagnosis.
Candidates for a hepatobiliary scan include individuals with:
- Unexplained abdominal pain: Especially in the upper right side of the abdomen.
- Suspected gallbladder disease: Such as cholecystitis (gallbladder inflammation).
- Jaundice: Yellowing of the skin and eyes due to a blockage in the bile ducts.
- Biliary obstruction: Suspected blockage in the bile ducts that affects bile flow.
- Post-surgical complications: After gallbladder surgery to check for bile leakage or obstruction.
- Assessment before gallbladder removal surgery: To confirm gallbladder function.
- Suspected bile reflux: When bile is abnormally flowing back into the stomach.
Patients who are pregnant or breastfeeding should consult their doctor before undergoing a hepatobiliary scan, as radiation exposure should be minimised. Additionally, individuals with severe liver disease or allergic reactions to radiotracers may require alternative diagnostic methods.
Benefits of a Hepatobiliary Scan
- Noninvasive and safe: The procedure involves a small amount of radiation, is generally well-tolerated, and does not require surgery.
- Real-time imaging: Unlike other imaging methods, this method assesses organ function dynamically over time rather than providing a still image.
- Early detection of gallbladder disease: It helps diagnose conditions like gallbladder inflammation before they become severe.
- Accurate assessment of bile duct function: It can identify biliary obstructions, strictures, or leaks that may not be visible on ultrasound or CT scans.
- Evaluation of gallbladder emptying: Measures how effectively the gallbladder releases bile, which can help diagnose biliary dyskinesia (a motility disorder of the gallbladder).
- Detection of bile leaks after surgery: Particularly useful in patients who have had gallbladder removal (cholecystectomy).
- Guides treatment decisions: Helps doctors decide whether gallbladder removal or other necessary interventions.
Conditions Diagnosed by a hepatobiliary scan
A hepatobiliary scan is primarily used to diagnose and evaluate conditions affecting the liver, gallbladder, and bile ducts, including:
Gallbladder Conditions
- Acute cholecystitis (gallbladder inflammation)
- Chronic cholecystitis
- Gallbladder dyskinesia (biliary dyskinesia)
Bile Duct Disorders
- Biliary obstruction
- Bile leakage
- Primary sclerosing cholangitis (PSC)
Liver Conditions
- Hepatitis
- Liver transplant evaluation
Post-Surgical Complications
- Bile duct injury after surgery
What Further Information Can a Hepatobiliary Scan Show?
In addition to diagnosing conditions like gallbladder inflammation and bile duct blockages, a HIDA scan offers the following insights:
- Bile Flow and Emptying Rate: The scan measures how efficiently bile moves from the liver to the gallbladder and intestines.
- Gallbladder Ejection Fraction (EF): Determines how well the gallbladder contracts and empties bile into the small intestine. A low ejection fraction (<35%) suggests biliary dyskinesia.
- Differentiation Between Obstruction and Dysfunction: Helps distinguish between mechanical obstructions (e.g., gallstones, tumours) and functional disorders (e.g., biliary dyskinesia).
- Post-Surgical Evaluation: Detects bile leaks or post-operative complications after gallbladder removal or liver surgery.
- Liver Function Insights: Though not a primary liver test, this test can indicate hepatocellular dysfunction, which means the liver is not effectively processing and excreting bile.
Preparation for a Hepatobiliary Scan
Proper preparation ensures accurate scan results. Below are the key guidelines:
What to Bring
- Referral Letter: If required by the imaging centre.
- Medications List: Inform the radiologist about any medications you take, especially opioids, anticholinergics, or prokinetics, as these can affect bile flow.
- Identification & Medicare/Insurance Details
What to Wear
- Loose, comfortable clothing (without metal zippers or buttons) is recommended.
- You may need to change into a hospital gown.
- Minimal jewellery
Eating & Drinking Instructions
- The patient must have something to eat 3 hours before the test and then fast until the test is completed.
Medication Guidelines
- Avoid opioids for 24 hours before the scan (e.g., morphine, codeine, tramadol), as these can slow bile movement and affect scan accuracy.
- Certain medications may need to be paused or adjusted only under a doctor’s guidance.
Time Required
- The scan usually takes 1–2 hours, but sometimes, it may take up to 3 hours if delayed imaging is needed.
- Allow extra time in your schedule in case additional images are required.
Hepatobiliary Scan Procedure
Arrival & Preparation
- You will check in at the imaging centre and provide any necessary paperwork.
- A technologist will explain the procedure and answer any questions.
- You may be asked to change into a gown.
Radiotracer Injection
- A small amount of a radioactive tracer (Technetium-99m HIDA) is injected into a vein in your arm.
- This tracer travels through the bloodstream to the liver, where it is absorbed and released into bile.
Imaging with a Gamma Camera
- You will lie on a scanning table, and a gamma camera positioned over your abdomen will take images at regular intervals.
- The camera detects the radiotracer's movement through the liver, gallbladder, bile ducts, and intestines.
- The scan may last 60–90 minutes, but if bile movement is slow, additional images may be taken.
What to Expect After a Hepatobiliary Scan?
Immediate Aftercare
- You can resume normal activities immediately unless sedatives or pain medications were given.
- Drink plenty of fluids to help flush the radioactive tracer from your body.
- You may be advised to eat a light meal to help stimulate bile flow.
Results & Follow-Up
- A radiologist will analyse the images and prepare a report for your doctor.
- Results will be available the following day after 2pm.
- Your doctor will discuss the findings and recommend any necessary treatment or further testing.
Hepatobiliary Scan Prognosis
Early detection of gallbladder and bile duct issues through a hepatobiliary scan leads to timely treatment and a good prognosis for most conditions.
Hepatobiliary Scan Risks
The scan is generally well-tolerated, but some patients may experience:
- Mild discomfort at the injection site
Radiation Exposure Precautions
- The radiation dose is very low and typically does not pose a risk.
- However, if you are pregnant or breastfeeding, inform the doctor beforehand.
- Breastfeeding mothers: You may be advised to pause breastfeeding for 24 hours to allow the tracer to leave your body.
What if a Hepatobiliary Scan is Delayed?
Delaying a HIDA scan may impact the diagnosis and management of gallbladder, bile duct, or liver conditions, especially if a patient is experiencing significant symptoms.
When Should a HIDA Scan Be Done Urgently?
A hepatobiliary scan should not be delayed if you experience:
- Severe right upper abdominal pain (especially after meals).
- High fever and chills (possible gallbladder infection).
- Persistent nausea and vomiting.
- Jaundice (yellowing of skin and eyes).
If these symptoms occur, an urgent scan and evaluation are recommended.
Hepatobiliary Scan Costs
Medicare Coverage
Bulk billed. No out-of-pocket cost.



